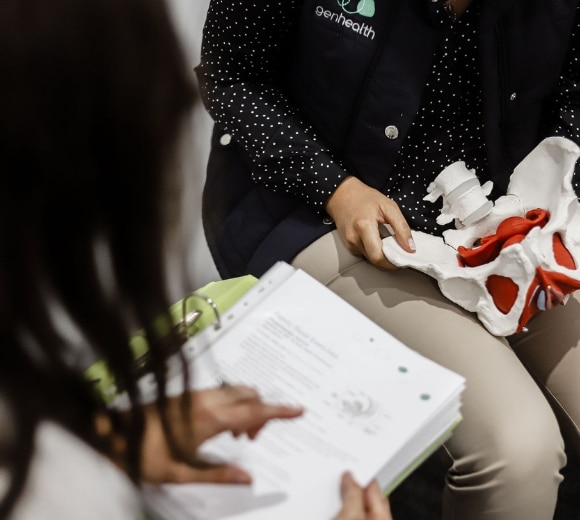
Pelvic Health Physiotherapy
At Gen Health, we are fortunate to have experienced pelvic health physiotherapist, Jessica. Jessica has completed and stays up to date with postgraduate education to provide this very important service to our region

At Gen Health, we are fortunate to have experienced pelvic health physiotherapist, Jessica. Jessica has completed and stays up to date with postgraduate education to provide this very important service to our region

This appointment is designed for women and those who identify as non binary or trans male who were assigned female at birth. Jessica consults in an inclusive, safe and trauma informed practice always.
Urinary Incontinence – symptoms include feelings of likely bladder leakage or actual bladder leakage. For example, the incontinence may be associated with coughing, laughing, sneezing or also may be associated with urgency: the sudden unexplained rush to need to get to the toilet.
Bowel dysfunction – this may include symptoms of constipation or faecal incontinence, or somewhere in between.
Pelvic Pain – this can include menstrual pain, pain with intercourse or arousal, pain with exercise, painful bladder syndrome, frequent and recurrent UTI and thrush infections.
Pelvic Organ Prolapse – often described as symptoms of heaviness or dragging sensations into the vagina, it may be associated with low back pain or symptoms of incomplete emptying of the bladder and/or bowel.
Pregnancy – everything from pelvic girdle pain, pubic symphysis dysfunction, safe exercise during pregnancy, pregnancy related low back pain, pregnancy related carpal tunnel and other pregnancy musculoskeletal conditions.
Postpartum – optimising your recovery after birth, recovery of birth trauma and birth injuries, safe return to exercise postpartum.
Mastitis– using lymphatic drainage techniques and therapeutic ultrasound to assist with the treatment of inflammation associated with mastitis.
As pelvic health physiotherapists, we will complete a full subjective assessment with you. With your consent, we will ask you questions about your bladder health, your bowel health, your gynaecological health and obstetric history.
We may ask about your sexual experience if it is relevant. We have a number of tools to objectively assess your presentation. These include but are not limited to: bladder and bowel diaries, suprapubic ultrasound of the pelvic floor muscles, external palpation and internal vaginal examination.
As with any physiotherapy assessment and treatment, we discuss your options with you and ensure you feel comfortable with every stage of the assessment and treatment process.

Yourself! If you have a referral from your GP or gynaecologist, please let us know at the time of booking. We may also get you to complete the Pelvic Floor Questionnaire – so please check your emails prior to your appointment. If you are coming for mastitis management, we encourage you to bring your bub to feed immediately after treatment.
You do not have to have any assessment you do not feel comfortable with. We have a number of tools in our toolkit to help form a diagnosis and management plan.
No. You can self refer by booking online or calling the friendly reception team. We do receive referrals from GPs, gynaecologists, maternal child health nurses and midwives just to name a few.



132 Thompson Street,
Hamilton, Victoria 3300
Monday – 8am – 6pm
Tuesday – 8am – 7:30pm
Wednesday – 8am – 7:30pm
Thursday – 8am – 6pm
Friday – 8am – 5:30pm
We acknowledge the Gunditjmara people as the traditional custodians of the lands on which we live & work and all first nations people on country who have contributed to the diverse Aboriginal Society we have today and in to the future.
We respect the rich culture & history and are committed to working towards reconciliation and a strong future for all.